When a person has diabetes, their body can have difficulty producing or using insulin so wound healing may be delayed. Several complications may result from this delay, including infections that can be fatal or lead to amputations.
Typically, the healing process for diabetic wounds can take anywhere from a few weeks to several months, depending on the wound's severity and overall health.
In this blog post, we will explore the different factors that can affect the healing time for wounds, especially those dealing with diabetes, and how we can speed up the healing process.
How Long Does A Diabetic Wound Take To Heal: 6 Factors
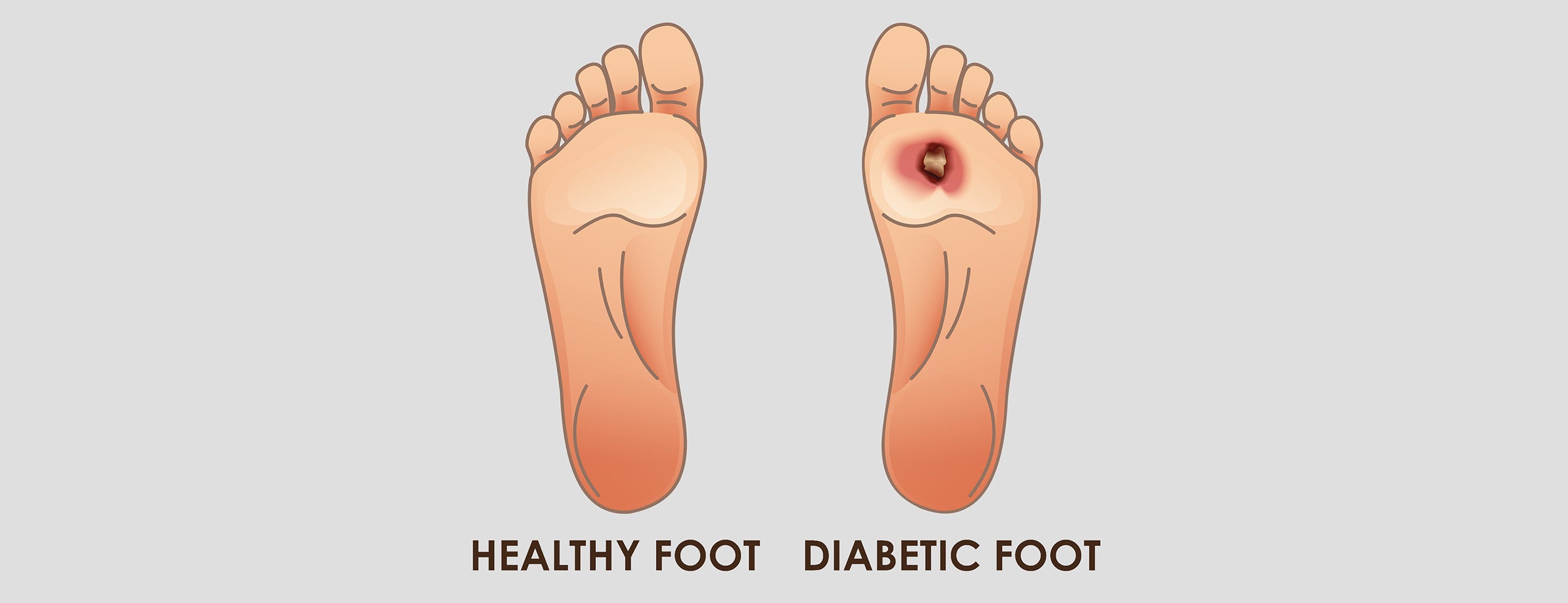
A diabetic wound's healing time depends on several factors, including its severity, the individual's health, and wound management. Diabetes tends to affect circulation, neuropathy, and immunity, slowing wound healing.
High Blood Sugar Levels:
High blood sugar levels can delay the healing of diabetic wounds. A high glucose level in the blood can damage nerves and blood vessels. The longer the blood sugar levels remain high, the longer it takes for the wound to heal. Maintaining healthy blood sugar levels can accelerate healing.
Blood sugar levels must be maintained within a healthy range by managing diabetes properly, including diet and exercise. Monitoring blood sugar levels and seeking medical attention for wound-related complications can prevent delays.
Poor Circulation:
Poor circulation can decrease oxygen supply to the affected area, inhibiting the body's natural healing process. People with diabetes often have poor circulation, which contributes to slow wound healing. The immune response may be negatively impacted by prolonged wound healing in diabetics.
When circulation is poor, essential nutrients cannot reach wounds, hindering healing. Wound healing requires adequate circulation, and patients with chronic conditions affecting circulation may have a higher risk of slow healing. Medical attention and managing underlying conditions can improve circulation and speed up healing.

Immune System Deficiency:
Diabetes patients' immune systems can be compromised, resulting in delayed wound healing due to fewer and less effective immune cells. This can lead to prolonged inflammation and an increased risk of infection. It takes diabetic wounds twice as long to heal as non-diabetic wounds.
Poor blood circulation and nerve damage in people with diabetes also contribute to delayed wound healing. Proper wound care and treatment can reduce the risk of complications and promote faster healing.
Wound Size And Depth:

Wound size and depth are crucial factors in determining the healing time for diabetic wounds. The larger and deeper the wound, the longer it will take to heal. Blood vessel growth and wound healing are affected because glucose cannot be metabolized properly.
Usually, deep wounds are healed by debridement, which involves removing dead tissue. Also, large wounds may require more frequent dressing changes and additional wound care.
Infection And Complications:
Diabetic wounds are more likely to become infected, which can significantly slow down the healing process. Therefore, keeping the wound clean and appropriately dressed is crucial to prevent infection. Infection and complications can prolong the healing time of diabetic foot ulcers.
Diabetes can slow the healing process and make wounds more susceptible to infection. Infection can lead to more serious complications, such as cellulitis and osteomyelitis. Diabetic foot ulcer healing is highly affected by the treatment plan and severity of the wound.
Patient's Age And Overall Health:
The patient's age and overall health are crucial in healing diabetic wounds. The healing process may be delayed in older adults with cardiovascular disease, neuropathy, or impaired immunity. Diabetes can cause vascular and nerve damage, leading to slower healing.
Diabetic wounds can take 12 weeks to heal, longer if the patient has comorbidities or poor glucose control. Wound care, glycemic control, and comorbidities must be addressed for optimal healing.
Phases of Diabetic Wound Healing
Diabetic wound healing involves three phases: the inflammatory phase (immune response and debris removal), the proliferative phase (tissue regeneration and angiogenesis), and the maturation phase (collagen remodeling and scar formation). These sequential stages collectively contribute to wound closure and tissue restoration.
Inflammatory Phase:

The inflammatory phase is the initial stage of wound healing, during which the body's immune system clears debris and pathogens. This phase typically lasts 1-5 days, but in diabetic wounds, it can last much longer due to impaired immune function.
Due to this prolonged inflammatory state, diabetic wounds can take significantly longer to heal and often develop into chronic wounds. Diabetes-related foot ulcers can take several months to years to heal, requiring aggressive interventions such as surgery and advanced wound care.
Diabetic wounds should be closely monitored, and aggressive treatment plans should be implemented early in the healing process to prevent chronic wounds.
Proliferative Phase:
During the proliferative phase of diabetes, growth factors stimulate the division of cells and collagen synthesis, which facilitates the repair and regeneration of tissues.
The duration of the diabetic proliferative phase varies from 4 to 21 days, depending on the severity of the wound and the individual's ability to heal.
Diabetes can lead to a prolonged proliferative phase and increased infection risk due to impaired blood flow, nerve damage, and compromised immune function.

Maturation Phase:
The remodeling of tissue and the strengthening of the wound characterize the maturation phase of wound healing. This phase typically lasts between 21 days and two years, depending on the severity and location of the wound.
During the maturation phase of diabetic wounds, maturation factors are deficient, causing a delay in healing and an increased risk of chronicity. Diabetic wounds heal in different amounts of time, depending on the patient's condition and wound care.
Duration of Diabetic Wound Healing
Diabetic wound healing takes weeks to several months, depending on factors such as wound type, health, and complications. Diabetic-related factors can significantly influence the healing process.
The Size of The Wound:
The size of the wound is a significant factor in determining how long a diabetic wound takes to heal. Generally, the larger the wound, the longer it takes to heal. Some large wounds may take over six months to heal completely.
Smaller wounds may heal within a few weeks as long as they are given proper care and treatment. Diabetic patients must monitor their wounds closely and seek medical attention if they notice any size, color, or discharge changes.
Locations of The Wound:

The location of the wound also plays a crucial role in determining how long it takes to heal. Diabetic wounds on the legs and feet often take longer to heal than elsewhere because blood flow is reduced in these areas.
This lower blood flow means healing cells and nutrients take longer to reach the wound. The increased pressure on the foot from walking or standing may also impede the healing process.
Treatment Applied To The Wound:
A diabetic wound heals at a different pace depending on several factors, including severity, overall health, and treatment effectiveness.
- Clean the wound thoroughly with mild soap and water.
- Apply an antibiotic cream or ointment to prevent infection.
- Cover the wound with a sterile dressing or bandage.
- Elevate the affected area to reduce swelling and promote blood flow.
- Manage blood sugar levels through diet, exercise, and medication.
- Use specialized wound dressings, such as hydrocolloids or foam dressings, to promote healing.
- Undergo debridement, the removal of damaged tissue, if necessary.
- Receive hyperbaric oxygen therapy, which can accelerate healing by increasing oxygen flow to the wound.

Physical Activity And Lifestyle Choices:
A diabetic wound can also take longer to heal due to physical activity and lifestyle choices. Physically active diabetics can heal faster than those who don't exercise or consume unhealthy foods.
Taking too much alcohol, smoking, and not sleeping enough causes the body to heal wounds more slowly. The physical activity and lifestyle choices of diabetic patients must be carefully monitored.
Conclusion
In conclusion, diabetic wound healing time is influenced by various factors, including the size and location of the wound, the treatment applied, and lifestyle choices.
Previously untreated wounds will take longer, and early intervention is recommended. Effective wound care practices and a healthy lifestyle can help minimize the time required for healing.
Diabetic patients need to take good care of their wounds and follow a consistent wound treatment plan to prevent further complications. Further research is needed to continue advancing treatment options and improving wound healing outcomes for diabetic patients.